Pinched Nerve Physio
Physio for a Pinched Nerve in the Lower Back
By Aaron Woolley, Physiotherapist
Experiencing a nagging pain in your lower back that extends to your buttocks or down your leg? You might be dealing with a pinched nerve that physio can help with. This pain can often be incredibly horrible and cause a lot of fear and concern for the people who experience this condition. At Robina Physio on the Gold Coast, our physiotherapists often see patients from across the Gold Coast area struggling with the discomfort of lower back pain and pinched nerves. Here’s how to identify, manage, and alleviate your symptoms effectively.
What Is a Pinched Nerve in the Lower Back?
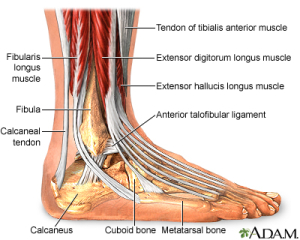
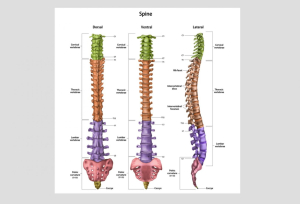
A pinched nerve occurs when there’s compression or irritation of the nerve roots in your lumbar spine. You might feel sharp or burning pain, typically radiating along your sciatic nerve. This condition, commonly known as sciatica, generally affects just one side of the body.
Common Symptoms Include:
- Back Pain
- Muscle Spasm
- Pins and needles
- Numbness
- Weakness in your leg
- Burning or tingling sensations
- Reduced reflexes
Symptoms can occasionally affect the front of your thigh and hip, referred to as femoral nerve compression.
What Causes a Pinched Nerve?
Many factors contribute to nerve compression, such as:
- Herniated or bulging discs
- Spinal stenosis (narrowing)
- Degenerative disc disease
- Facet Joint Arthritis
- Spondylolithesis
- Incorrect lifting techniques
Other factors can also produce similar pain and impact a pinched nerve such as, long periods of sitting, repetitive bending and muscle spasm/tightness, especially the Quadratus Lumborum and Piriformis muscles. Given that up to 90% of Australians experience back pain at some stage, addressing the underlying cause is crucial for long-term relief.
Physio Advice To Relieve Pinched Nerve Pain
Initial pain relief strategies include:
- Applying heat or ice packs
- Practicing good posture/bending to ease spinal stress
- Avoiding extended periods of sitting or inactivity
- Regular gentle movements throughout the day
- Limiting heavy lifting and intense physical activity during the acute stage
- Consulting with a qualified physiotherapist at Robina Physio on the Gold Coast for tailored advice and industry-leading treatment
Physio Stretches for Pain Relief
Incorporating specific stretches can significantly relieve nerve compression and associated lower back pain. Below are a few examples of common exercises we may prescribe at Robina Physio on the Gold Coast to help manage your pinched nerve and associated lower back pain.
-
Piriformis Stretch
- Lie on your back with one leg crossed over the other.
- Gently pull the crossed knee toward the opposite shoulder.
- Hold for 20 seconds, repeating five times on each side.

Image credit: VALD MoveHealth
-
McKenzie Extension
- Be careful not to push this exercise too hard or it might make your pain worse.
- Lie face down, propped on your elbows.
- Slowly push up with your arms, allowing your back to gently arch.
- Hold briefly and repeat five times.

Image Credit: VALD MoveHealth
-
Cat/Cow Exercise
- Begin on hands and knees, ensuring alignment of knees under hips and wrists under shoulders.
- Alternate between rounding your spine upwards (cat) and arching it downwards (cow).
- Flow gently between poses, repeating five times.

Image Credit: VALD MoveHealth
-
Core Strengthening
Strengthening your core can provide excellent spine support and alleviate nerve pain:
- Engage in gentle core exercises like planks, side planks, bridges, and controlled abdominal movements (avoid any exercise that exacerbates pain and start small).

Image Credit: VALD MoveHealth
Regular walking and gentle mobility exercises also significantly benefit nerve pain management. Aim to gradually increase your walking tolerance.
Also check out some of our previous blogs that may help manage your lower back pain and sciatica…
Physio For Low Back Pain In Golf
Dry Needling & Acupuncture In Lower Back Pain
Expert Physio Assessment at Robina Physio
At Robina Physio on the Gold Coast, we specialise in providing accurate diagnosis and personalised treatment plans for pinched nerves and lower back pain. Our experienced physiotherapists will assess your condition thoroughly, relieve your acute symptoms, and recommend effective, tailored exercises for ongoing relief.
Ready to tackle your back pain and get moving pain-free again? Our physio team is here to help you regain mobility and live a healthier, pain-free life on the Gold Coast.
Book Your Physio Appointment Online Now at Robina Physiotherapy