Achilles Pain
Achilles Pain
By Aaron Woolley, Physiotherapist.
Achilles Pain is a common complaint affecting large numbers of people in the community. The most common injury encountered is termed Achilles Tendinopathy. An overuse injury that involves a range of pathological alterations in the Achilles tendon, often resulting from prolonged overuse and chronic excessive strain on the tendon. This condition is observed in both athletes and non-athletes and may occur with or without an accompanying Achilles tendon tear. Reduced flexibility or stiffness in the Achilles tendon can heighten the risk of such injuries.
What is the Achilles Tendon?
The Achilles tendon holds the title of the largest and most robust tendon in the human body, endowed with the ability to withstand substantial tensile loads. This tendon emerges from the lower union of the gastrocnemius and soleus muscles and anchors into the lower part of the heel bone, known as the calcaneus.
Encasing the Achilles tendon is a structure called the paratendon, functioning like an elastic sheath that grants the tendon the liberty to glide amidst the neighbouring tissues. However, the vascular supply along the tendon’s length is relatively deficient, as evidenced by the scant count of blood vessels per unit of cross-sectional area. This is particularly true for the segment situated 4-6 cm above the heel bone. Such limited blood flow is often associated with longer healing times after sustaining an injury.
What is a Tendinopathy?
Tendinopathy can be depicted as existing on a spectrum. Progressing along this spectrum, one encounters a robust and healthy tendon, which can transition into a reactive tendinopathy stage. This stage further evolves into tendon disrepair and eventually leads to a degenerative tendon. A tendon’s position on this spectrum is influenced by the loads it endures, and this position can fluctuate based on different factors.
Clinically, tendinopathy is often described as a tendon’s unsuccessful attempt at healing. This condition involves abnormal growth in tenocytes (the cells of a tendon), disturbances within these cells, a breakdown in the collagen fibres, and an increase in the non-collagenous substances within the tendon. The term “tendinopathy” is a general term used for conditions linked to tendon overuse, which includes both the experience of pain and pathological changes. Moreover, tendinopathy is marked by pain, reduced functional ability, and a decreased tolerance for exercise.
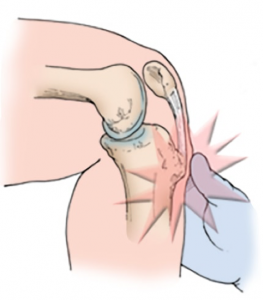
Achilles Pain (tendinopathy) can be categorised as either insertional or mid-portion, distinguished primarily by the location of the condition. Insertional Achilles tendinopathy occurs at the junction where the Achilles tendon meets the bone, specifically within 2 cm of its insertion point. In contrast, mid-portion Achilles tendinopathy is found in the body of the tendon, more than 2 cm away from where it attaches to the bone.
Causes of Achilles Pain (Tendinopathy)
The precise cause of Achilles Tendinopathy remains unclear. Achilles pain is often thought of as an injury that only affect sports people. But in-fact this injury is also often found in people who do not practice sports. What we do know is that Achilles tendinopathy is caused from both intrinsic and extrinsic factors. The causes and mechanisms include:
Intrinsic factors: Age, sex, metabolic dysfunction, muscle weakness/imbalance, gastrocnemius dysfunction, anatomical variation of the plantaris muscle, tendon vascularization, torsion of the Achilles tendons and lateral instability of the ankle.
Extrinsic factors: Include mechanical overload, constant effort, inadequate equipment, obesity, medications (corticosteroids, anabolic steroids, fluoroquinolones), improper footwear use, insufficient warming or stretching and sharp changes in training loads.
Achilles Pain Presentation and Assessment
Pain experienced in the morning is a signature symptom, as the Achilles tendon is required to endure a complete range of motion, including stretching, right after rising in the morning. Typically, symptoms are concentrated in the tendon itself and the adjacent area. Swelling of the Achilles tendon is not common but in chronic cases the tendon may become thickened at the tendinopathy site.
When assessing Achilles Pain, a thorough subjective examination gives many key clues to the mechanism of injury. On objective examination palpation of the tendon is one of the most useful tests. A positive result would result in pain, +/- thickening of the tendon of the site. Other important examination components include, range of motion, strength testing, anatomical and technique analysis and special tests including the arc sign and Royal London Hospital Test.
Imaging studies are not essential for diagnosing Achilles Pain (Tendinopathy) but can be beneficial for distinguishing it from other conditions. Ultrasound stands out as the preferred imaging method because it clearly reveals the tendon’s dimensions, variations in the tendon’s water content and collagen structure, as well as any swelling in the bursa. If the diagnosis is uncertain or if the symptoms do not follow the typical pattern, an MRI might be recommended.
At Robina Physio on the Gold Coast, we work closely with GP’s, Sports Physicians and Orthopaedic Specialists. This collaboration is especially important in more severe cases that may require more intensive treatments that are available such as PRP injections and in rare cases surgery. Our aim is to provide comprehensive care and support to address your Achilles issues effectively and get you walking and running again pain free.
Achilles Pain (Tendinopathy) Treatments
Treating tendon issues is the bread and butter of any physio. At Robina Physio on the Gold Coast we use highly effective treatment techniques and get fantastic results for managing Achilles pain. Treatment techniques we use includes:
- Load Management: As this injury is mostly impacted by over loading of the Achilles, this is perhaps the most important factor when managing Achilles pain. Finding the “sweet spot” of load is important, followed by gradually increasing tendon loads within the Achilles limits.
- Strengthening Exercises / Tendon Loading: Used in conjunction with load management, gradually loading the Achilles in a specific manner is key to stimulating a healing response within the tendon. Typically, we start with isometric holds, then progress into isotonic contractions with progressively increasing loads that match the sport specific needs of the tendon.

- Technique Correction: Poor biomechanics are a common problem related to Achilles pain. These poor biomechanics may need shoe adjustments but also often require running technique assessment and correction. At Robina Physio on the Gold Coast we have highly experienced running physios that offer in depth running and footwear analysis.
- Soft Tissue Release: Maintaining the balance of muscles in the leg e.g. gastrocnemius and soleus are an important adjunct to managing Achilles pain. Tightness in the lower limb is often present in people with Achilles pain.
- Dry Needling: Is another highly effective adjunct treatment Robina Physio on the Gold Coast offers. In many cases a combination dry needling the leg muscles and threading the Achilles tendon to help relieve pain and promote healing is highly effective.

Achilles Pain Physio Gold Coast
I hope you found this information helpful. The Physiotherapists at Robina Physio are highly experienced and highly trained in the management of Achilles pain. If your struggling with Achilles Pain and Tendinopathy please don’t hesitate to Contact Us on (07) 5578 7233 or BOOK ONLINE.